One of the most important steps for prevention is to be alert to any risk factors you may have for osteoporosis and broken bones. Knowing what your risk factors are will help you to take action to reduce bone loss and encourage you to request testing if needed.
What are osteoporosis risk factors?
A risk factor is anything that increases your chance of getting a disease. Having one or more risk factors does not mean that you will have osteoporosis. However, the more risk factors you have, the greater your chance of developing the disease.
Bone loss due to osteoporosis happens without any symptoms. The only two ‘visible’ signs that may suggest that you have osteoporosis include:
These are signs of possible spine fractures (your doctor may call them ‘vertebral fractures’). Spine fractures are often extremely painful, but sometimes aren’t. In that case, height loss and curved back may be the only tell-tale signs.
In most cases a doctor will recommend diagnostic testing depending on your age and if you have other risk factors for the disease. See diagnosis.
Below is a list of other common risk factors, some of which can be changed, and others which cannot.
The older you are, the more likely you are to have osteoporosis. Around 75% of fractures due to osteoporosis happen in people aged 65 and over.
Women are more likely to develop osteoporosis than men.
You are at greater risk if your parents had osteoporosis or a broken hip.
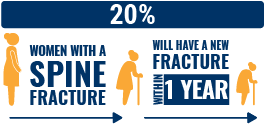
If you’ve broken a bone after a minor fall, this is a sign that you may have osteoporosis.
Oestrogen has a protective effect on bone, and with menopause women start to lose bone at a faster rate. That’s why women who have early menopause (before age 45) or have had a hysterectomy, are at greater risk.
Medications
Certain medications have side effects that are linked to osteoporosis or increased fracture risk. These include:
- Long-term glucocorticoid therapy: these medications (e.g. prednisone) are often used to treat arthritis or asthma. Using glucocorticoids for three months or more places you at higher risk of fracture.
- Certain steroid hormones (medroxyprogesterone acetate, luteinising hormone releasing hormone agonists) and hormone deprivation therapy (androgen deprivation therapy)
- Proton pump inhibitors
- Certain medications to treat diabetes
- Certain antidepressants, anxiolytics, sedatives and neuroleptics
- Certain immunosuppressants (calmodulin/calcineurin phosphatase inhibitors)
- Thyroid hormone treatment (L-Thyroxine)
- Aromatase inhibitors (used to treat breast cancer)
- Certain chemotherapy agents
- Certain antipsychotics
- Certain anticonvulsants, anti-epileptics
- Anti-coagulants
Other diseases
Some diseases may weaken bones and increase the risk of osteoporosis and fractures. Among these, the more common diseases and disorders are:
- Rheumatoid arthritis (note: this is a major and common risk factor!)
- Nutritional/gastrointestinal problems (lactose intolerance, Crohn’s, inflammatory bowel, coeliac disease, etc.)
- Chronic obstructive pulmonary disease (COPD) and asthma
- Endocrine disorders including hypogonadal states (diabetes, Cushing’s syndrome, hyperparathyroidism, Turner/Klinefelter syndrome, amenorrhea, etc.)
- Immobility
- Chronic kidney disease
- HIV/AIDS
- Cancers (including prostate and breast cancer)
- Haematological disorders
- Psychophysiological disorders and mental illness (dementia, anorexia nervosa)
Excessive alcohol intake
Drinking more than 2 units of alcohol per day increases the risk of fracture.
Smoking
Smoking almost doubles the risk of hip fracture compared to risk in non- smokers.
Low body mass index
Maintaining a healthy body weight is important - and being underweight with a BMI below 19 is a significant risk factor.
Poor nutrition
A diet rich in calcium, protein, fruits and vegetables benefits bone health. ‘Malnutrition’ is a major concern in seniors who are at greater risk of falls and fractures as a result.
Vitamin D deficiency
Low levels of vitamin D are common, particularly among seniors who do not go outdoors, or in the winter months in northern latitudes.
Eating disorders
Disorders such as anorexia or bulimia can result in extreme weight loss, which is dangerous for bone health. In young women, this results in estrogen deficiency (much like menopause) and very low calcium intake, with resulting rapid bone loss.
Inactivity (not enough exercise)
Lack of exercise results in bone (and muscle) loss. Adults who are inactive are more likely to have a hip fracture than those who are more active.
Low dietary calcium intake
Calcium is a very important nutrient for bone health. With age, the body’s ability to absorb calcium declines, which is one of the reasons why seniors also require higher amounts.
Frequent falls
People who have a tendency to fall are at higher risk of fracture. Read more about preventing falls.
Read more information about risk factors in our brochure ‘Know your risk factors’.
You can find out if you have risk factors for osteoporosis by taking the IOF ‘Osteoporosis Risk Check’ that you can find on this website.